State-of-the-Art Zirconia Solutions for Dental Prosthetics

The use of zirconia-based dental restorations has revolutionized the way modern dentists think about restorative options, material selection and appropriate material application. The availability of a tooth-colored indirect restorative material with favorable intraoral durability, esthetics and functional properties offers patients additional treatment options. However, dental professionals must understand appropriate application of this unique material and, perhaps more importantly, the material’s strengths and weaknesses in each application. This issue of Prosthodontics Newsletter reviews several recently published studies that discuss the profession’s advancing understanding of this unique material.
Improving the Esthetics of Zirconia Restorations
Monolithic yttria-stabilized tetragonal zirconia poly- crystal (Y-TZP) restorations have high flexural and mechanical strength, cause minimal wear to opposing teeth, take less time to fabricate, do not need veneering porcelain and cost less than other alternatives. The esthetics of Y-TZP restoration, however, can be a problem. While clinicians cannot control the intrinsic factors, such as material microstructural and processing properties, that affect color and translucency, they can manipulate those external factors that are under their control to increase the restoration esthetics. Pekkan et al from Tekirdag Namık Kemal University, Turkey, reviewed the clinical factors influencing the monolithic Y-TZP ceramics translucency to create the most esthetically pleasing result.
Thickness: Because thickness in versely affects zirconia translucency, a thinner restoration is generally preferable. Y-TZP restorations can be as thin as 0.5 mm to 0.9 mm, without compromising strength or color.
Cement: Resin cements and resinmodified glass ionomer cements yield higher translucency values than do conventional glass ionomer cements. Cement color can be classified as shaded, bleached, opaque or transparent. Opaque cements mask dark, metal or discolored backgrounds but will require an increase in zirconia thickness of 0.9 mm to 1.6 mm to compensate. With tooth-colored backgrounds and cements, the need to use a thicker zirconia is minimized.
Color: Zirconia blanks may be pre shaded by the manufacturer or externally shaded at the time of fabrication to match surrounding teeth. Because zirconia translucency depends on the material type, the shading technique chosen depends on the type of zirconia chosen.
Finishing: Monolithic zirconia manufacturers recommend application to a polished or glazed surface, polished carefully to avoid creating defects and scratches that would negatively impact survival. Glaze firing appears to eradicate compressive stresses.
Low-temperature degradation (LTD): LTD refers to the changes zirconia undergoes over time from water and low temperature. As the zirconia restoration ages, it loses translucency. Partially cubic monolithic high-translucent or multilayered zirconia may not be subject to the same LTD as standard Y-TZP. These newer formulations have lower strength and toughness, and require great care when placed.
Comment
Translucency is a major contributor to the creation of an esthetically pleasing zirconia restoration. The practitioner can control thickness, cement, material color and surface finish to create the best es- thetic result.
Pekkan G, Özcan M, Subaşı MG. Clinical factors affecting the translucency of monolithic Y-TZP ceramics. Odontology 2019;doi:10.1007/s10266-019-00446-2.
Zirconia Restorations In Bruxism Treatment
Severe bruxism can cause extensive attrition and erosion; these patients may re quire extensive functional and esthetic rehabilitation of the full dentition. One possible treatment involves increasing the vertical dimension of occlusion, which maximizes space for restorative material and the amount of tooth displayed, while minimizing the need for invasive procedures.
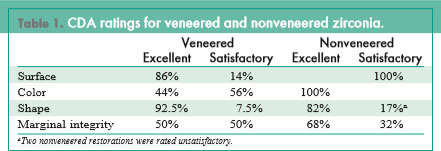
The preferred treatment uses high-strength monolithic zirconia restorations because of their resistance in high–load-bearing areas, despite their esthetic inferiority to fully veneered zirconia crowns. But the difference in outcomes between these 2 restorations has not previously been investigated. Levartovsky et al from Tel Aviv University, Israel, conducted a retrospective study to evaluate the clinical performance of buccally veneered and nonveneered zirconia restorations in bruxism patients un- dergoing increased vertical dimension of occlusion.
Ten patients with bruxism (aged 62–70 years) were treated with complete rehabilitation using increased vertical dimension of occlusion. Nonveneered zirconia was used for final restorations in posterior quadrants, while final restorations in the anterior quadrants, especially in the maxilla, received feldspathic ceramic veneers on nonfunctioning buccal surfaces.
After a mean period of >2 years, 250 restorations (108 veneered, 142 nonveneered) were evaluated for surface, color, shape and marginal integrity us ing a modified California Dental Association (CDA) quality evaluation system with 4 grades:
- excellent
- satisfactory
- unsatisfactory-reparable
- unsatisfactory-irreparable
Comment
The increase in vertical dimension of occlusion ranged from 2 mm to 7 mm. Only 1 restoration failed. All surfaces in the nonveneered group were rated excellent, as were all but 14% of surfaces in the veneering group; the remaining surfaces were rated satisfactory due to minor chipping that required only polishing to repair. Nearly all restorations were graded satisfactory or excellent in all 4 criteria evaluated (Table 1).
Levartovsky S, Pilo R, Shadur A, et al. Complete rehabilitation of patients with bruxism by veneered and non-veneered zirconia restorations with an increased vertical dimension of occlusion: an observational case-series study. J Prosthodont Res 2019;63:440-446.
Zirconia Complete Denture With New Nanocomposite Framework
When all-acrylic-resin maxillary complete dentures require reinforcement, they typically receive a framework of cobalt-chromium (Co-Cr). Fabricating Co-Cr frameworks can be complicated, and some pa tients are allergic to this alloy. A newly developed complete denture with a framework of ceria-stabilized zirconia–alumina nanocomposite may solve these patients’ problems.
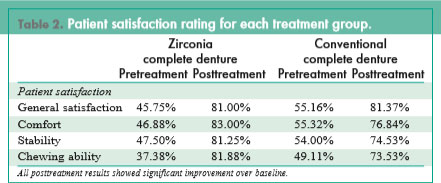
Nishiyama et al from Showa University School of Dentistry, Japan, compared the clinical performance of the zirconia maxillary complete denture with conventional maxillary complete dentures. A total of 29 patients (10 with the zirconia denture, 19 with conventional dentures; mean age, 75 years) were followed for a mean of >2 years during which no denture fractures occurred. At the 12-month followup, satisfaction scores increased significantly from baseline in both groups for general satisfaction, comfort, stability and chewing ability with no significant differences in satisfaction scores between the 2 groups (Table 2).
Comment
This small first study showed that maxillary complete dentures with zirconia nanocomposite frameworks may be a promising and ef fective treatment option for edentulous patients.
Nishiyama H, Tanaka S, Nemoto R, et al. Zirconia-reinforced framework for maxillary complete dentures. Int J Prosthodont 2018;31:114-116.
Bonding Strength Of Universal Adhesive Systems
The high metal oxide content of crystalline ceramics gives these materials excellent mechanical strength but hinders bonding procedures. Two universal adhesive systems claim to facilitate bonding to zirconia without the drawbacks of previous systems. dos Santos et al from Universidade de Pernambuco– UPE, Brazil, compared the bonding strength of these new materials with that of a zirconia primer and tested their effectiveness with both polished and grit-blasted zirconia surfaces.
Eighty zirconia blocks were divided into 2 groups (polished and gritblasted with aluminum oxide par ticles); 10 of each group then re ceived an application of 1 of 4 ad- hesive systems:
- Scotchbond Universal (3M ESPE), a universal adhesive system
- All Bond Universal (Bisco), a universal adhesive system
- Z-Prime Plus (Bisco), a zirconia primer
- Z-Prime Plus + All Bond Universal
Each block was topped with cylindrical composite resin buildups and stored for 24 hours before undergoing microshear bond strength testing and analysis using scanning electron microscopy (SEM).
All systems performed similarly and displayed significantly greater bonding strength on grit-blasted surfaces than on polished surfaces. On polished surfaces, the universal adhesive systems significantly outperformed the zirconia primer, which failed to achieve a clinically adequate bond strength. SEM revealed a distinct difference between polished and grit-blasted surfaces at the adhesive interface.
Comment
One limitation of this study was that it analyzed only the immediate bond strength of the tested materials without simulating clinical and longevity conditions. However, the study does suggest the bonding quality of the new universal adhesive systems bond to zirconia is as good if not better than that of zirconia primer.
dos Santos RA, de Lima EA, Mendonça LS, et al. Can universal adhesive systems bond to zirconia? J Esthet Restor Dent 2019;doi:10.1111/jerd.12521.
Suitability Of Zirconia Abutments with Bonded Titanium Inserts
Zirconia abutments create less mucosal discoloration, an important esthetic consideration when choosing a restoration. They also have been used outside the esthetic zone in premolar and molar areas. Two main designs exist: a 1-piece zirconia abutment, which has demonstrated a low fracture resistance and causes wear of implant fixtures, and a 2-piece zirconia abutment made up of a zirconia sleeve and a titanium insert.
Lin et al from Chang Gung Memorial Hospital, Republic of China, conducted a retrospective and clinical follow-up study to evaluate the outcome of implant restorations supported by 2-piece zirconia abutments with bonded titanium inserts. Records of 32 pa tients with 36 implant-supported restorations supported by 50 zirconia abutments placed at their medical center from 2008 to 2013 were reviewed. All patients were adults in good health with either natural teeth or fixed tooth- or implantsupported restorations opposing the restoration site.
Of the original cohort, 27 patients attended a recall examination be- tween January and December 2017 (mean follow-up time, 6.6 years). All implants remained fully integrated; however, 7 zirconia abutments in 4 patients failed. Fractures of the zirconia sleeve and the ti- tanium insert occurred in 4 abutments; fracture of the zirconia sleeve only occurred in 1 abut- ment. Two other restorations suffered debonding between the zirconia sleeve and the titanium insert, and 1 failed 3 different times.
Statistical analysis showed a significant relationship between abutment failure and abutment location: 6 of the 13 abutments placed in posterior areas but only 1 of the 29 abutments placed in anterior areas failed. All fractures occurred in molars treated with 1 particular implant system that did not create a complete metalto-metal implant–abutment connecting platform. Of the 3 patients with bruxism, 2 suffered multiple fractures of the zirconia sleeve and titanium insert; 1 patient devel oped porcelain chipping at the distal marginal ridge of the ceramic crown; 1 patient developed periimplantitis; 9 patients developed peri-implant mucositis.
Comment
This study suggested that 2-piece zirconia abutments with bonded titanium inserts can be a suitable treatment option for teeth in the esthetic zone. But these zirconia abutments, which do not have a complete metal-to-metal connection platform, may not be suitable for use in the molar area.
Lin Y-T, Shen Y-F, Wei P-C, Hsu K-W. Clinical evaluation of two-piece zirconia abutments with bonded titanium inserts for implant-supported restorations. J Prosthet Dent 2019;doi:10.1016/j.prosdent.2019.01.006.


 (425) 549-4649
(425) 549-4649